The Kentucky Core Healthcare Measures Set (KCHMS) was established in 2018 as a mechanism to collect and monitor healthcare quality measures in Kentucky and Kentuckiana. The current KCHMS is a set of 42 primary care measures that were developed with the intent to align measurement efforts in the Commonwealth towards shared areas of focus. The development of the first KCHMS was led by the KHC, alongside many diverse community partners, using a consensus-based process. Past KCHMS committee members have included representatives from Humana, Kentucky Primary Care Association, Foundation for a Healthy Kentucky, CHI St. Joseph, Kentucky Department for Public Health, and Norton Healthcare. Every two years, the KCHMS is updated to ensure that measures reflect current priorities. The overall goals of the KCHMS are to:
- Improve the quality and value of care by focusing attention on measures that are meaningful and broadly applicable;
- Reduce provider reporting complexity;
- Align Kentucky’s healthcare organizations around a common set of quality measures.
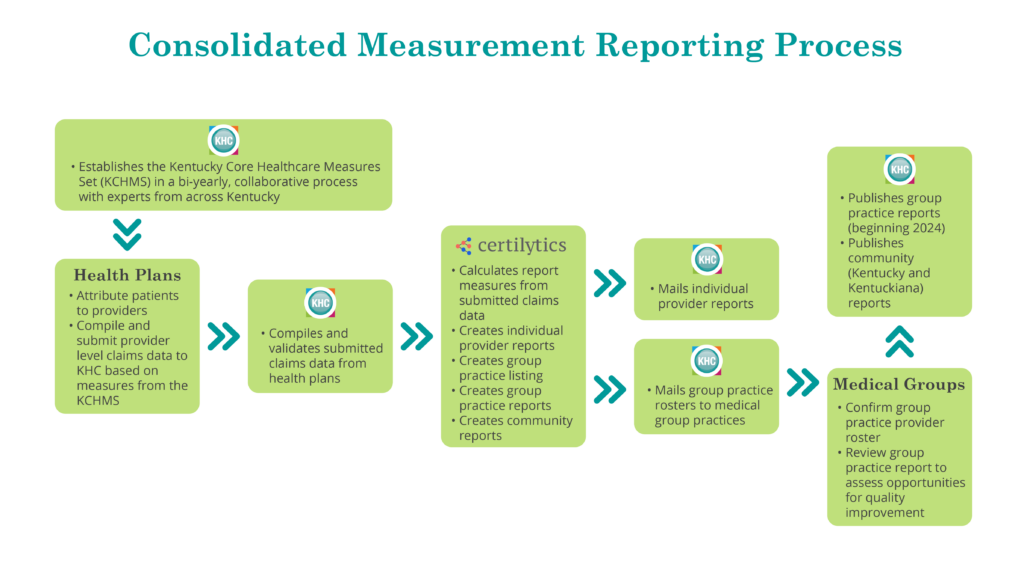
The KCHMS is the foundation for the KHC’s Consolidated Measurement Reporting (CMR). Each year, the KHC works with our health plan partners (Aetna Better Health of Kentucky, Anthem Blue Cross Blue Shield, Humana Health Plan of Kentucky, Molina Healthcare of Kentucky, and WellCare Health Plan of Kentucky) to collect aggregate measures from commercial and Medicaid health plan claims data to create three reports which focus on measures captured in the KCHMS. These reports are:
- Individual Provider Reports: These reports are mailed each year to more than 5,000 individual healthcare providers in Kentucky and Kentuckiana. These reports are intended to increase provider awareness of the quality of care they are providing in their own practice, and to serve as a foundation for quality improvement activities. These reports are not publicly available.
- Group Practice Reports: These reports are mailed each year to more than 500 group practices in Kentucky and Kentuckiana. These reports aggregate quality measures at the group practice level and are, again, intended to increase awareness of the quality of care being provided at group practices. Currently, these reports are not publicly available but, beginning in 2024, KHC intends to post the results of these reports on our website.
- Community Reports: These reports are made available on KHC’s website each year and reflect the quality of care provided in both Kentucky and Kentuckiana. The most recent Kentucky and Kentuckiana reports can be found on our website.
We recently created a flow chart that illustrates the entire process of the CMR and we encourage you to take a look and reach out if you have questions.
This fall, the KHC will launch the next update of the KCHMS with the goal of having an updated measures set available in late spring/early summer 2024. The updated measures will guide the CMR data collection in future years. In the fall, KHC will open a nomination process to recruit individuals and organizations interested in serving on the Oversight Committee or one of the five Subcommittees (Preventive Care, Behavioral Health, Pediatric Care, Chronic and Acute Care, Cost, Utilization, and Experience) that will be required to update the KCHMS. We hope that you can join us in this important endeavor. Stay tuned for more information and, as always, reach out if you have questions or want to discuss the KHC’s measurement work. We are looking forward to convening partners across the state to support this important effort in early 2024!