The Kentuckiana Health Collaborative is a data-driven organization. For more than 15 years, we’ve led the way in driving healthcare quality and value of care through our measurement and transparency work, primarily through our annual quality healthcare reports. We know that you can’t truly address an issue without first understanding its components, often revealed through data. And this fall, the KHC dived deeply into data as part of our continued partnership in the Kentucky Opioid Response Effort (KORE), partnering with national data leaders to explore opioid use trends for Kentucky’s residents.
This fall, the KHC partnered with IBM Watson Health to develop benchmarks for key metrics related to the prevention, treatment, and recovery of opioid misuse and opioid use disorder. IBM Watson Health derived these benchmarks from MarketScan, a fully integrated drug and medical claims database that includes more than 350 carriers and 25% of U.S employer-sponsored healthcare beneficiaries. The benchmarks are specific to Kentucky and represent 22% of the state’s two million commercially insured members, ranging in age from 18 to 64. The claims covered service dates from January 2016 to December 2017 and were compared alongside national averages.
In November 2019, experts from IBM Watson presented the key findings and recommended next steps in a webinar to 44 attendees, including the opioid employer cohort and KHC members. Compared to national figures, the Commonwealth had a 12% higher opioid utilization rate in 2017, and while Kentucky saw a 4% decrease from 2016, national rates decreased by 8%.
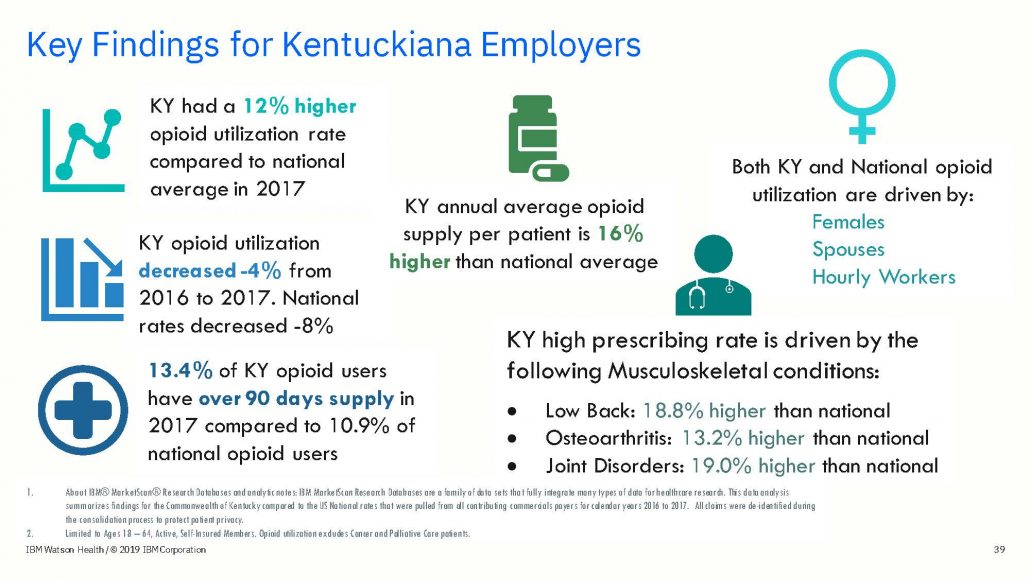
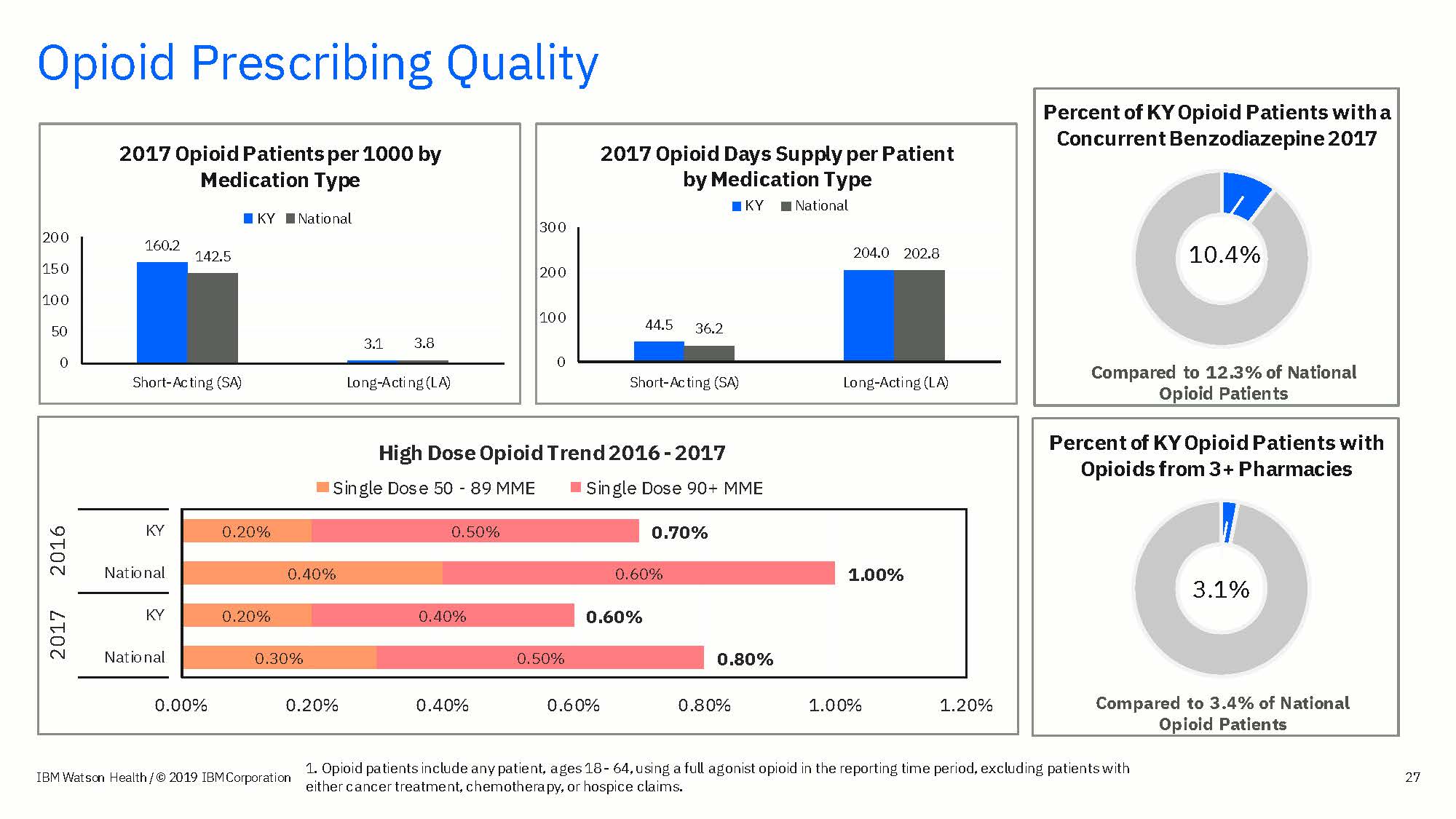
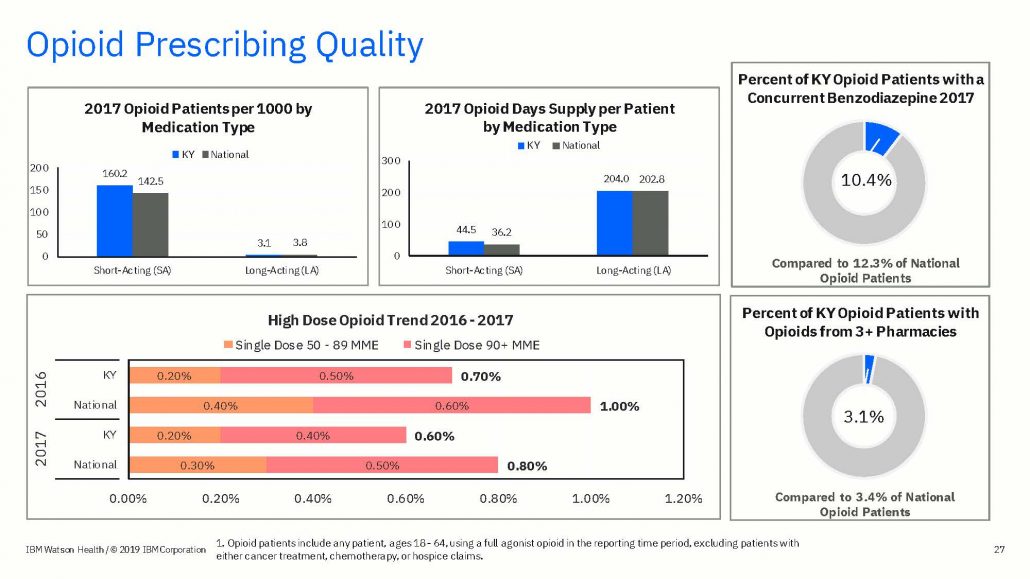
In Kentucky, 8% of opioid users accounted for 62% of the opioid supply in 2017, and half of those individuals received enough supply to cover more than 360 days in the year, meaning they likely had overlapping prescriptions. In fact, the Kentucky annual average opioid supply per patient was 16% higher than the national average. While Kentucky received longer supply of opioids, they had lower utilization of high-dose opioids, meaning that the strength of the opioids prescribed was lower.
On the opioid abuse treatment side, Kentucky showed very positive results for use of medication assisted treatment (MAT), demonstrating higher prevalence of and adherence to MAT. Kentucky patients overall were less expensive for opioid abuse treatment.
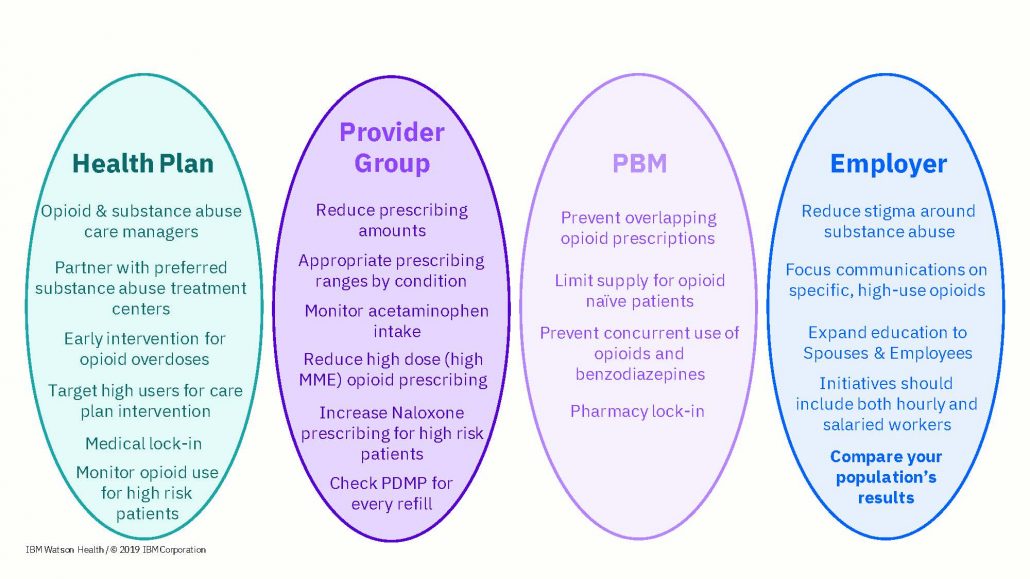
In the webinar, IBM Watson outlined 18 key next steps for Kentucky’s employers, ranging from reducing stigma and expanding education to medication benefit design reform.
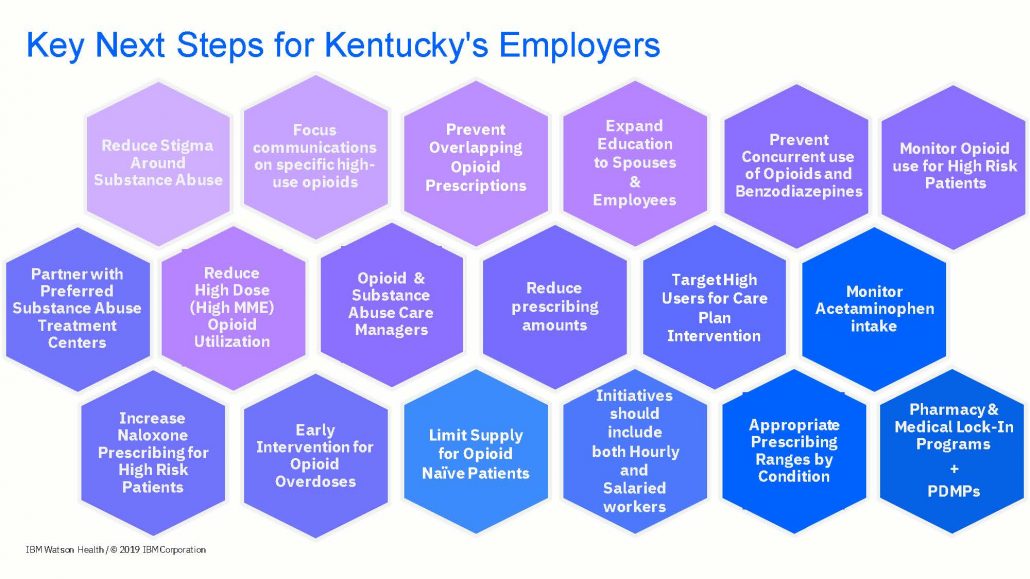
While 18 items to focus on might seem overwhelming, those items were categorized into the entity which is appropriate to take the lead on each of those items: either with health plans, provider groups, PBMs, or employers.
So how can employers utilize this data? For employers who can access their own data, the benchmarks are useful tools for them in determining where they lie. Are they above or below the average? Is this a positive or negative indicator? What changes can be made in response? For employers who do not have access to their data, the benchmarks can provide useful insight into Kentucky’s workforce and serve as loose representations of their own.
If interested in learning more detail about this data and key takeways, a recording of our November webinar can be viewed here. In the coming months, the KHC will be utilizing these benchmarks to develop resources for employers to be included in the Opioids and the Workplace toolkit. If you are an employer interested in learning more about how to retrieve or interpret your data, please contact Natalie Middaugh at nmiddaugh@khcollaborative.org or Stephanie Clouser at sclouser@khcollaborative.org for assistance.