Last week’s Community Forum focused on diabetes care in our Kentuckiana region. At the Forum, we got to hear the best practices of providers who are providing benchmark-level care for their patients with diabetes. To kick off the morning, the KHC team (with the help of many of our partners) put together an infographic on priorities for diabetes prevention, care and control in our region.
Last week’s Community Forum focused on diabetes care in our Kentuckiana region. At the Forum, we got to hear the best practices of providers who are providing benchmark-level care for their patients with diabetes. To kick off the morning, the KHC team (with the help of many of our partners) put together an infographic on priorities for diabetes prevention, care and control in our region.
We have a unique perspective at the KHC, since we work with many different stakeholders – payers, providers, employers and consumers. Our stakeholders help lead our focus, and that is reflected in the Five Priorities we have outlined for diabetes.
Although priority is labeled with a number (it is a list, after all!), they are not listed in order of importance. Rather, it is imperative that we address all of these priorities to improve outcomes in diabetes care.
Five Priorities for Diabetes in Kentuckiana
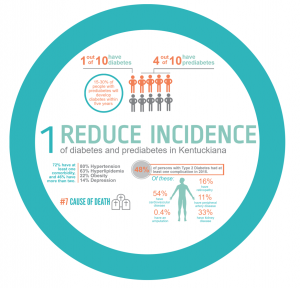 Our first priority is to reduce Incidence of diabetes and prediabetes rates in Kentuckiana. Nationally, one in 10 individuals has diabetes. Here in the Kentuckiana region, one in 10 people also has diabetes, but the local rate is slightly higher than the national rate, 10.8 percent in Kentuckiana compared to 9.3 percent nationally. On top of that, 37 percent of the U.S. population has prediabetes, and 90% of those estimated 86 million people don’t even know they have it. And without lifestyle changes, 15 to 30 percent of people with prediabetes will develop type 2 diabetes within the next five years. Prevention is key with these folks.
Our first priority is to reduce Incidence of diabetes and prediabetes rates in Kentuckiana. Nationally, one in 10 individuals has diabetes. Here in the Kentuckiana region, one in 10 people also has diabetes, but the local rate is slightly higher than the national rate, 10.8 percent in Kentuckiana compared to 9.3 percent nationally. On top of that, 37 percent of the U.S. population has prediabetes, and 90% of those estimated 86 million people don’t even know they have it. And without lifestyle changes, 15 to 30 percent of people with prediabetes will develop type 2 diabetes within the next five years. Prevention is key with these folks.
Diabetes is the seventh most common cause of death in Kentuckiana, and we know that there are many deaths that are related to diabetes but not necessarily attributed to diabetes. Comorbidities include hypertension, hyperlipidemia, obesity and depression, and nearly half of individuals with type 2 diabetes in Kentuckiana had at least one complication last year.
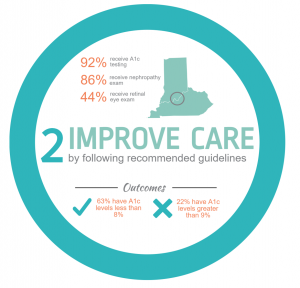 We also want to improve the care that patients with diabetes receive, including receiving recommended screening for A1c (average level of blood sugar over the past two to three months), nephropathy and retinopathy. Diabetes is the number one cause of blindness in Kentucky, and just 44 percent of individuals with diabetes in Kentuckiana receive the recommended retinal eye exam for detecting and monitoring retinopathy.
We also want to improve the care that patients with diabetes receive, including receiving recommended screening for A1c (average level of blood sugar over the past two to three months), nephropathy and retinopathy. Diabetes is the number one cause of blindness in Kentucky, and just 44 percent of individuals with diabetes in Kentuckiana receive the recommended retinal eye exam for detecting and monitoring retinopathy.
Looking at the “benchmark” providers in the area (the top performing docs who make up the care for 10 percent of the population for each measure), A1c screening and nephropathy screening rates are 100 percent, compared to region’s total rate of 92 percent and 86 percent for A1c and nephropathy screenings, respectively. Eye exam rates for the benchmark providers are 67 percent.
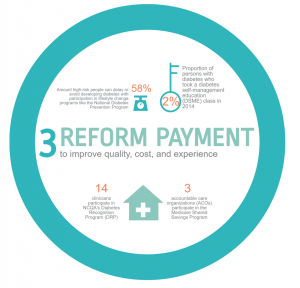 Our next priority is to reform payment to improve quality, cost and experience. Payment reform isn’t about just paying for things – it’s about changing incentives to improve quality while wisely using resources and paying for services not currently covered, such as using care managers, registered dieticians, social workers, etc., that improve diabetes care. One way to do that is through patient education. The National Diabetes Prevention Program (DPP) can reduce the risk of developing diabetes by 58 percent, but few patients have this as a covered benefit. The Kentucky Employer Health Plan is an exception (they cover about 265,000 members). Medicare will cover DPP in 2018. There are only three organizations in the area that participate in Medicare’s Shared Savings Program. Our understanding is that there is only one organization in the area that is applying under Medicare Access and CHIP Reauthorization Act (MACRA) as an Advanced Alternative Payment Model. We believe payment reform is critical to improving diabetes care. We know that many of the services that are needed to improve care are not currently paid for in the fee-for-service world.
Our next priority is to reform payment to improve quality, cost and experience. Payment reform isn’t about just paying for things – it’s about changing incentives to improve quality while wisely using resources and paying for services not currently covered, such as using care managers, registered dieticians, social workers, etc., that improve diabetes care. One way to do that is through patient education. The National Diabetes Prevention Program (DPP) can reduce the risk of developing diabetes by 58 percent, but few patients have this as a covered benefit. The Kentucky Employer Health Plan is an exception (they cover about 265,000 members). Medicare will cover DPP in 2018. There are only three organizations in the area that participate in Medicare’s Shared Savings Program. Our understanding is that there is only one organization in the area that is applying under Medicare Access and CHIP Reauthorization Act (MACRA) as an Advanced Alternative Payment Model. We believe payment reform is critical to improving diabetes care. We know that many of the services that are needed to improve care are not currently paid for in the fee-for-service world.
 Affordable solutions are imperative to manage costs and improve outcomes in diabetes. The Health Care Cost Institute (HCCI) recently released the 2015 Health Care Cost and Utilization Report, which showed that national spending per privately insured person grew by 4.6 percent – faster than in previous years. HCCI indicates that healthcare costs have increased three times faster than wages over the past decade and continues to strain government, employer and family budgets. According to the report, Kentucky had higher than national average out-of-pocket spending.
Affordable solutions are imperative to manage costs and improve outcomes in diabetes. The Health Care Cost Institute (HCCI) recently released the 2015 Health Care Cost and Utilization Report, which showed that national spending per privately insured person grew by 4.6 percent – faster than in previous years. HCCI indicates that healthcare costs have increased three times faster than wages over the past decade and continues to strain government, employer and family budgets. According to the report, Kentucky had higher than national average out-of-pocket spending.
Consumers throughout the region are feeling the strain. And this is amplified for individuals with diabetes, who have more than 3.5 times the healthcare spend of their neighbors without diabetes. The Health Care Incentives Improvement Institute (HCI3) and Catalyst for Payment Reform(CPR) Report Card on State Price Transparency Laws gave Indiana and Kentucky an “F” in transparency.
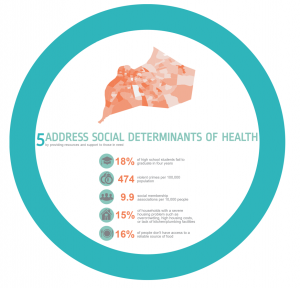 Our final priority, but certainly not the least important, is to address social determinants of health by providing resources and support to those in need. Most of us know why this makes our priority list for diabetes outcomes. An estimated 80 percent of what impacts a person’s health is outside the clinical care they receive. In order to address diabetes, you have to address health equity. Where you live matters when it comes of diabetes outcomes, including mortality. Zooming in on just Jefferson County, for which we have detailed information from the Louisville Metro Department of Public Health and Wellness (LMPHW), many of the neighborhoods with high diabetes mortality are also neighborhoods with socioeconomic challenges. Dr. Sarah Moyer, medical director for LMPHW, and Dr. Brandy Kelly Pryor, director of the Center for Health Equity at LMPHW, suggested that we look at education, food and housing security, and community safety among some of the most important factors to look at when examining the effect of social determinants of health. Some providers, including some we heard from at last week’s Community Forum, are beginning to make those community-clinical linkages to unmet social needs.
Our final priority, but certainly not the least important, is to address social determinants of health by providing resources and support to those in need. Most of us know why this makes our priority list for diabetes outcomes. An estimated 80 percent of what impacts a person’s health is outside the clinical care they receive. In order to address diabetes, you have to address health equity. Where you live matters when it comes of diabetes outcomes, including mortality. Zooming in on just Jefferson County, for which we have detailed information from the Louisville Metro Department of Public Health and Wellness (LMPHW), many of the neighborhoods with high diabetes mortality are also neighborhoods with socioeconomic challenges. Dr. Sarah Moyer, medical director for LMPHW, and Dr. Brandy Kelly Pryor, director of the Center for Health Equity at LMPHW, suggested that we look at education, food and housing security, and community safety among some of the most important factors to look at when examining the effect of social determinants of health. Some providers, including some we heard from at last week’s Community Forum, are beginning to make those community-clinical linkages to unmet social needs.
Final thoughts
Those are some of the data points that we, with a great amount of help from our partners, identified to illustrate where our gaps are and where we are doing well as a community. Now we want your feedback. Which of these priorities are you most interested in focusing on? What is your organization doing around these priorities? Where do you see the greatest opportunity for improvement? Fill out this form and let us know.
Really, we put this together to help focus our attention to areas where we can concentrate to have better diabetes outcomes in Kentuckiana. With greater healthcare transparency, we can manage costs. With better care, we can reduce complications such as retinopathy and amputations. And with a focus on patient education, we can delay or even prevent a diabetes diagnosis.
Last week we heard the personal story of Jeri McCullough, who in 2009 was diagnosed with type 2 diabetes and struggled with her weight, a sedentary lifestyle, and out-of-control eating habits. But in 2014, she was hit with some harsh realities, when her eyesight was altered and a trip to the doctor revealed scary blood sugar levels. Jeri took control of her health, involved her family, and today her A1c levels are under control and her diabetes is controlled without the use of medication. If we focus our attention to the right areas, such as the ones we have outlined above, we can have many more Jeri stories.