When it wrapped up its 2023 legislative session, the Kentucky General Assembly missed a vital opportunity to take an important step in tackling one of the most significant issues facing the Commonwealth, its vital business sector, and its working families: the high and rising cost of health care. Let’s start with a few troubling facts.
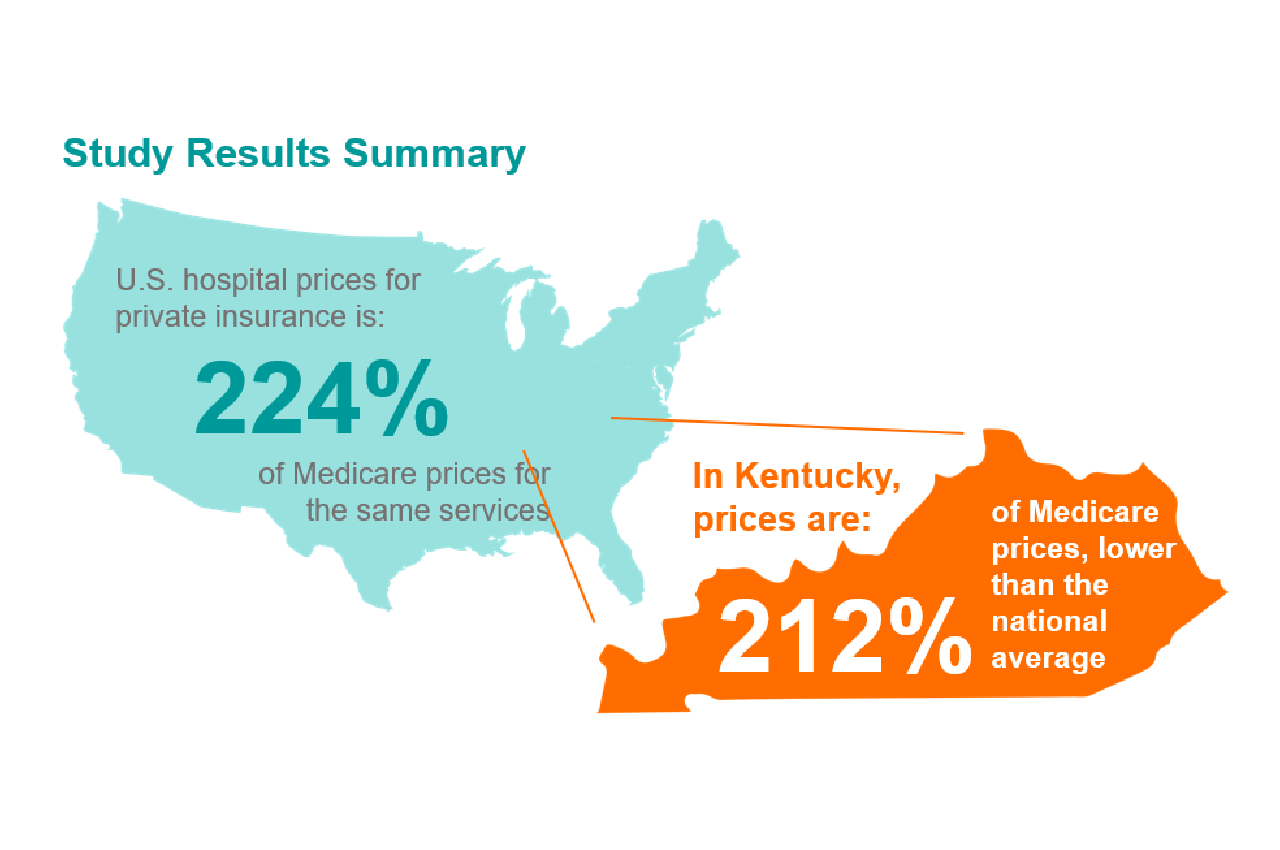
In 2020, healthcare spending in the United States increased by 10%, reaching $4.1 trillion. Healthcare now accounts for a whopping 20% of the United States economy – making one in every five dollars spent attributable to healthcare. While there are many causes for high and increasing health care costs, hospital prices are the leading driver of these costs in Kentucky and around the country. Hospital care makes up nearly four-in-ten dollars spent on healthcare each year. [1] According to the Health Care Cost Institute, between 2016-2020, inpatient hospital prices increased by 24.6 percent – a rate nearly three times higher than the price of healthcare professional services (9 percent), and substantially higher than prescription drug prices (15.8 percent). As prices increased during this period, total healthcare utilization decreased by 5.4 percent (with the decline in utilization beginning prior to the COVID-19 pandemic). [2]
In light of this, improving healthcare affordability has been one of the most urgent, and at times contentious, legislative issues for more than a decade at both the state and federal level – with meaningful breakthroughs requiring bipartisan support and collaboration. Despite acknowledgement from both sides of the aisle that these rising costs are unsustainable, progress often seems elusive. In March, a critical piece of legislation that could have helped lower these costs failed in Kentucky, keeping our state in the minority share of those that do not have an All-Payer Claims Database (APCD).
Rising costs are a national problem that hits close to home – more than 75% of Kentuckians fear being unable to afford basic healthcare in the future, making many reluctant to seek out care until conditions are acute and require hospitalization. Today, hospitalization is one of the most expensive and financially difficult situations a person can face. This need not be our reality. Too often, policymakers, employers, and everyday consumers are operating in a healthcare system that resembles a “black box,” where prices, out-of-pocket costs, and quality are difficult to decipher.
Lawmakers should focus on policy solutions rooted in data and provide constituents with enough information to make informed decisions on behalf of themselves and their employees. At Kentuckiana Health Collaborative, our values are in our name – we believe cross industry collaboration is essential to tackle rising costs and that policies put forth should consider all stakeholders impacted by the policy. When addressing high costs in our state, Kentucky policymakers have the opportunity to learn from the successes in other states that have yielded results for stakeholders.
One solution to help tamp down extreme hospital costs that has seen success in other states is an all-payer claims database (APCD). This database aggregates data reported from health insurers, both public and private, to offer detailed information on healthcare cost, utilization, and quality of care in the state. Claims reported include medical, pharmacy, and dental services. This public information would play a significant role in giving policymakers, researchers, employers, and consumers the facts they need to understand and reduce the rate of growth for healthcare costs, which have soared to over $20,000 per family in Kentucky –– a burden shared between employers and individuals. Kentucky has long prided itself on being “the most pro-business state in America” with low business costs, streamlined regulation, high quality of life and good infrastructure as key selling factors for the state. [3] Yet high and rising healthcare costs threaten this historically warranted bravado as unsustainable costs cut into both wages and profits as premiums continue to remain sky high.
The trends that have emerged from existing federal hospital transparency requirements have shown disturbing realities in the costs of care, both within states and across the nation. For example, hospital price transparency reporting has allowed researchers to find that joint replacements for knee and hip surgery cost an average of $58,193 in the New York metro area – more than double the average price in the Baltimore, MD region where the average is $23,170. [4] This variation also occurs within states, and among insurance carriers for almost every screening and procedure from lab tests to open heart surgery.
States use their APCD to monitor conditions uniquely impacting their communities and region. In Virginia, the state APCD operates a dashboard that tracks potentially avoidable emergency room visits – a notoriously expensive and common situation in our fractured health care system. These data can be compared across the state by county, health planning region, and insurance type over multiple years. [5] Using this information, policymakers can identify which hospitals and plans have the highest rate of avoidable emergency room visits, and craft policies to deter unnecessary visits or provide greater access to non-emergency providers.
In another instructive example, Colorado receives 20,000 visits annually to their Shop for Care site where consumers can search for average prices and quality of care at specific facilities for common procedures and imaging tests. These stats are also accompanied by ‘cost of care’ interactive reports and maps that show spending per person aggregated by year, age group, and type of payer for geographic regions of the state. [6] Armed with this knowledge, Coloradans are able to make the most informed and cost-effective choice for themselves and their families.
While essential to bring down costs, the data collected can also be utilized to inform public health policy, dissect health trends in a region, and track whether implemented policy reforms are working as intended. Aggregate data can show which health conditions have a disproportionate prevalence in certain areas, providing insight into where upstream and preventative care is needed, as well as interventions.
Minnesota adopted their all-payer claims database in 2008. Since its enactment, the database has been instrumental in both tracking and evaluating statewide initiatives including a one-time analysis of chronic pain management procedures, studying healthcare spending trends in chronic conditions, and more recently – a study on the impact of telehealth expansion and payment parity laws that took effect in 2021, with a full report due in 2024. [7]
There is considerable variation and flexibility in how different states fund, govern, and operate their APCDs. Some states opt for strict, binding reporting requirements, while others accept data from the providers and insurance companies on a voluntary basis. Funding comes from many different streams such as federal and state grants or appropriations. Governance is typically handled by a multi-stakeholder board, often appointed by state officials. As with any program, full compliance is difficult to obtain, as no initiative is perfect – however, this is a major step in demystifying costs and statewide trends. Federal law enacted at the end of 2021 provides grant funding to states to create or expand their APCDs and federal funds to help standardize this information, eventually linking databases and allowing for comparisons between states. A nationwide infrastructure of these price comparison tools holds the promise of reducing healthcare spending in the United States, while improving quality of care and creating a more equitable pricing framework.
By 2025 more than half of all U.S. states will have implemented an all-payer claims database. Unfortunately, Kentucky is not yet part of that majority. Several bills have been introduced in the legislature over the last few years, with none making it over the finish line. Wrangling out of control healthcare costs is a bipartisan priority, and APCDs have proven results as other states have successfully navigated the implementation of their own databases, with some boasting over a decade of use and meaningful change.
While a vital tool, APCDs – and transparency in general – are a necessary but not sufficient solution to solving our growing healthcare cost crisis. To leverage better transparency, however, policymakers should enact reforms that directly tackle many of the leading drivers of rising healthcare costs, including market consolidation, through laws that ban anti-competitive contracting and state price commissions. Kentuckiana Health Collaborative recently published a policy brief detailing the impact of high and rising hospital prices on Kentucky families and employers that outlines potential policy solutions.
We do not need to live in a reality where quality healthcare is difficult to come by and even more difficult to afford. While it is disappointing that an APCD was not approved by the legislature this year, Kentuckians still deserve common sense solutions to our rising healthcare costs. We encourage the legislature to prioritize introducing and passing measures related to an APCD when they are introduced in the next session. Kentuckians deserve transparency and fair pricing – we cannot afford to be left behind as other states make more equitable, high-quality care a reality in their communities.