Minority Health Month, held each year in April, is a time to learn more about the health status of racial and ethnic minority populations and to raise awareness of the health disparities that continue to affect racial and ethnic minorities. As an African-American female born with benign ethnic neutropenia, a blood disorder characterized by white blood cell counts that are persistently below the normal range of those with people of Caucasian descent, I adhere to suggested preventive clinical guidelines and annual health exams. A large proportion of healthy African-Americans have this blood disorder. With a family history of colon cancer, diabetes, and breast cancer, it is important for me to take personal responsibility for my health.
 In 2010, I started my doctoral degree in education and completed my dissertation, Predicting Adherence to Mammography Screening Practices among African-American Women, in 2014. I chose this topic because African-American women were disproportionately dying from breast cancer at a higher rate than other ethnic groups in Louisville, KY. You can see from the graph that there is a wide disparity between black Louisville residents and white Louisville residents in breast cancer deaths.
In 2010, I started my doctoral degree in education and completed my dissertation, Predicting Adherence to Mammography Screening Practices among African-American Women, in 2014. I chose this topic because African-American women were disproportionately dying from breast cancer at a higher rate than other ethnic groups in Louisville, KY. You can see from the graph that there is a wide disparity between black Louisville residents and white Louisville residents in breast cancer deaths.
Breast cancer is a leading cause of cancer death among women in the United States. According to the American Cancer Society, about 1 in 8 women will develop breast cancer and about 1 in 36 women will die from breast cancer. If look at current Jefferson County data, those statistics have improved overall and the disparity gap is narrowing. However, African-American women still have a higher death rate.
 According to the Susan G. Komen organization, overall nationally, breast cancer incidence (rate of new cases) is slightly lower among black women than among white women. However, breast cancer mortality is higher in black/African-American women. Lower screening rates in the past may be one possible reason for the difference in survival rates today. Black women now have slightly higher rates of mammography screening than other women. Even after accounting for differences in income, past screening rates, and access to care, black/African-American women are diagnosed with more advanced breast cancers and have worse survival than white American women. More research focusing on the differences in reproductive factors and breast cancer biology is needed to close the mortality disparity gap among African-American women and other ethnic groups. I proud to say that my sister is a 23 year breast cancer survivor!
According to the Susan G. Komen organization, overall nationally, breast cancer incidence (rate of new cases) is slightly lower among black women than among white women. However, breast cancer mortality is higher in black/African-American women. Lower screening rates in the past may be one possible reason for the difference in survival rates today. Black women now have slightly higher rates of mammography screening than other women. Even after accounting for differences in income, past screening rates, and access to care, black/African-American women are diagnosed with more advanced breast cancers and have worse survival than white American women. More research focusing on the differences in reproductive factors and breast cancer biology is needed to close the mortality disparity gap among African-American women and other ethnic groups. I proud to say that my sister is a 23 year breast cancer survivor!
Men, don’t stop reading! Minority Health Month focuses on all minorities, not just women. My father and sister are both living with Type 2 diabetes; my father has had two lower-limbs amputated. Members of some racial and ethnic minority groups are more likely to have diagnosed diabetes than non-Hispanic white individuals. The Centers for Disease Control and Prevention reported among adults, American Indians/Alaska Natives had the highest age-adjusted rates of diagnosed diabetes among all racial and ethnic groups examined.
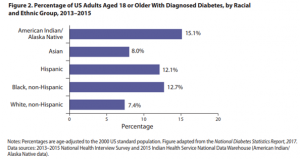 Diabetes-related complications can be serious, costly, and deadly. They include heart disease, stroke, kidney damage (chronic kidney disease and kidney failure), blindness, and amputations of the legs and feet. People with diabetes can better manage their condition and improve their health by following preventive care practices. These practices include receiving annual foot and eye exams and attending diabetes self-management classes.
Diabetes-related complications can be serious, costly, and deadly. They include heart disease, stroke, kidney damage (chronic kidney disease and kidney failure), blindness, and amputations of the legs and feet. People with diabetes can better manage their condition and improve their health by following preventive care practices. These practices include receiving annual foot and eye exams and attending diabetes self-management classes.
Kentucky has the seventh highest adult obesity rate in the nation, according to The State of Obesity: Better Policies for a Healthier America, released August 2017. Kentucky’s adult obesity rate is currently 34 percent, up from 22 percent in 2000 and from 13 percent in 1990. While Kentucky is trending in the wrong direction, black residents are leading the obesity figures. There are many socioeconomic reasons for this trend. Jefferson  County is trending in the right direction. The Louisville Metro Behavioral Risk Factor Surveillance Survey (BRFSS) for the 2016 measurement period, maintained by Louisville Metro Public Health, reported overall obesity rates at 31 percent, down from 33 percent in 2015.
County is trending in the right direction. The Louisville Metro Behavioral Risk Factor Surveillance Survey (BRFSS) for the 2016 measurement period, maintained by Louisville Metro Public Health, reported overall obesity rates at 31 percent, down from 33 percent in 2015.
Several of my friends have been diagnosed with prostate cancer. Prostate cancer develops mainly in older men, although it can affect women in very rare cases. The American Cancer Society reports about 1 man in 7 will be diagnosed with prostate cancer during his lifetime. What may be surprising is that race and ethnicity significantly influence who gets prostate cancer and who dies from it. African-American men have, by far, the highest incidence of the disease: they are roughly 1.6 times more likely 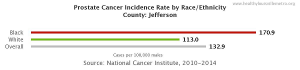 to develop prostate cancer than whites and 2.6 times more likely than Asian Americans. The gap in mortality rates is even more dramatic – African-Americans are more than twice as likely to die of prostate cancer as whites and about five times more likely to die of it than Asian-Americans. The high incidences of prostate cancer in African-American men holds true for those living in Jefferson County.
to develop prostate cancer than whites and 2.6 times more likely than Asian Americans. The gap in mortality rates is even more dramatic – African-Americans are more than twice as likely to die of prostate cancer as whites and about five times more likely to die of it than Asian-Americans. The high incidences of prostate cancer in African-American men holds true for those living in Jefferson County.
Health disparities affect everyone. Healthcare providers, policymakers, private sectors, and public sectors must all collaborate on initiatives to reduce disparities, advance equity, and strengthen the health and well-being of not only minorities, but all ethnic groups.