(Note: This guest post was written by Sarah Moyer, MD, MPH, director of Louisville Metro Department of Public Health and Wellness, and Lori Caloia, MD, medical director for Louisville Metro Department of Public Health and Wellness)
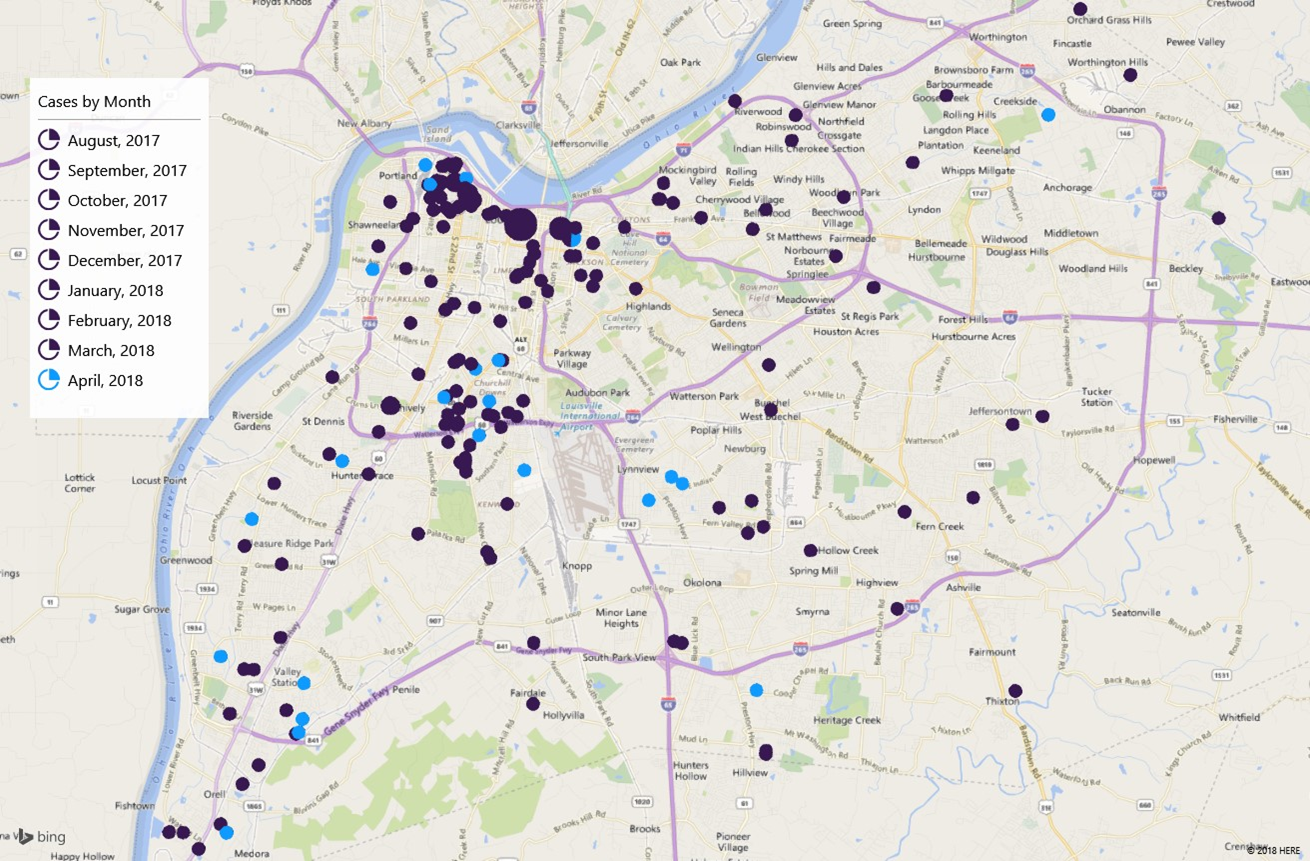
Louisville continues to work to control an outbreak of acute hepatitis A, which remains centered among the city’s homeless and those who use illicit drugs.
Hepatitis A is a vaccine-preventable, communicable disease of the liver caused by a virus. It is usually transmitted person-to-person through the fecal-oral route or consumption of contaminated food or water. Most adults with hepatitis A symptoms may experience fatigue, low appetite, stomach pain, nausea, or jaundice, that usually resolve within two months of infection; most children less than six years old and some adults do not have symptoms or have an unrecognized infection.
The best ways to prevent hepatitis A infection is to get vaccinated and to wash your hands frequently with soap and water, especially after using the bathroom or changing diapers and before eating or preparing food.
On November 21, 2017, the Kentucky Department for Public Health declared an outbreak of acute hepatitis A in several counties throughout the state, with the vast majority of cases in Louisville. The Louisville outbreak is epi-linked (shares the same genotype or genetic linkage) to a similar outbreak in San Diego, CA. Hepatitis A outbreaks are also occurring in Michigan and in Utah.
As of April 24, there had been 273 cases in Louisville with one death associated with the outbreak. There had been a total of three hepatitis A -associated deaths across the state. The Kentucky Department of Public Health has recommended that everyone living in counties affected by the outbreak be vaccinated. The Department of Public Health and Wellness continues to work with the Centers for Disease Control and Prevention (CDC) and the Kentucky Department for Public Health to provide vaccinations for those who use illicit drugs and for the homeless. Our vaccine is designated by federal regulation specifically for these groups.
The department and its community partners have given well more than 14,000 hepatitis A immunizations at homeless shelters, homeless camps, recovery houses and at agencies such as Family Health Centers’ Phoenix Health Center. It has also provided immunizations at Metro Corrections, both at intake and in the general population of inmates. It regularly continues to provide immunizations at its syringe exchange sites, its Specialty Clinic and at the MORE Center.
Others wishing to get hepatitis A immunization should check with their insurance company on where the insurer prefers that they go to get the vaccine and what, if any, cost might be associated with it. The vaccine is widely available at local pharmacies and health care providers.
Those who do not have health insurance, can be vaccinated at:
- Family Health Centers (several locations), 502-774-8631
- Shawnee Christian Healthcare Center, 234 Amy Ave., 502-776-1133
- Park DuValle Community Health Center (several locations), 502-774-4401
- Louisville Metro Department of Public Health and Wellness (no appointment needed), 400 E. Gray St., 502-574-6520,
- Monday; 8:00am – 5:00pm
- Tuesday, Wednesday, Friday; 8:00am – 12:00pm, 1:00pm – 5:00pm
- Louisville Metro Department of Public Health & Wellness Dixie Health Center (no appointment needed), 7219 Dixie Highway, 502-574-7975
- Monday, Wednesday, Friday; 8:00am – 12:00pm, 1:00pm – 5:00pm
Louisville has really come together to protect our out-of-town guests as well as residents during Derby festivities. Public Health and Wellness is teaming up with the U of L Global Health Clinic to offer below-cost immunizations to food service and hospitality businesses throughout the city. Thanks to donations from the Aetna and Anthem foundations, the cost has been reduced from $65 to $25 per dose. As of April 20, more than 1,100 food service workers from more than thirty businesses, including Churchill Downs vendors, had been immunized under this initiative. Businesses wishing to take advantage of this offer should call Dr. Ruth Carrico at 502 – 852-1324.
Like every year, the Department of Public Health and Wellness will be inspecting all food vendors at events like Derby, Oaks, and the Chow Wagons to make sure they are practicing safe food handling. While the outbreak remains centered among those who use illicit drugs and the homeless, the general population attending Derby events can protect themselves from hepatitis A by practicing good handwashing after using the restroom and before eating or drinking.
The Kentucky Derby Festival is posting signage at the various events to emphasize thorough handwashing. Hand sanitizer has been found to be not as effective as good handwashing at protecting against the hepatitis A virus, so the Derby Festival is installing hand washing stations at all events and has tripled the number of handwashing stations this this year over previous years.
The CDC has praised Louisville’s response to the hepatitis A outbreak, calling it the “gold standard” and a model for other cities to emulate.
Physicians and other healthcare providers can help to curb the spread of hepatitis A as follows:
- Expand your differential diagnosis. Think of hepatitis A in your patient work up, particularly if they have jaundice or the outbreak risk factors for hepatitis A of homelessness or drug use.
- Order a Hepatitis A IgM antibody test for confirmatory testing (a Hepatitis A Total Antibody does not help distinguish acute from prior infection or vaccination and should only be ordered to confirm immunity to HAV).
- Take a good history. Find out if infected patients have been in contact with anyone with hepatitis A, exactly when symptoms began (particularly jaundice, as this helps us to determine their infectious period in which they could have spread the virus to others), and where they have been living (i.e. homeless, correctional facilities or other congregate settings). Do they use drugs? Do they have other co-morbid diseases such as hepatitis B or C that may put them at risk for severe outcomes?
- Promptly report any suspected or laboratory confirmed case of Hepatitis A to LMPHW. Call communicable disease staff at (502) 574-6675 or fax EPID-200 form to (502) 574-5865. All communicable diseases are reportable to the health department (acute Hepatitis A within 24 hours) and the sooner we receive this information, the more time we have to contact the case patient, identify their contacts and provide post-exposure prophylaxis to contacts, further preventing disease. Please don’t rely on someone else to do this. The hospital lab reporting is often delayed. You, who are caring for the patient, are the first to suspect and often the first to respond to the positive lab result. The infection prevention nurse at your hospital can help with the reporting.
- Recommend hepatitis A vaccination to your patients! As a routine preventive health measure, HAV vaccine is covered by insurance. It is an incredibly effective vaccine, with 96 – 100% seroconversion within 4 weeks of vaccination. Even one dose of vaccine can be effective for up to 10 years and completion of the 2-part vaccine series confers 20 or more years of immunity.
- Provide post-exposure prophylaxis (PEP) to those who have been in contact with someone infected with HAV within 14 days of exposure. Healthy people age 1-40 should be provided Hepatitis A vaccine for PEP. Provide Immunoglobulin (IG) to close contacts of those with HAV if under age 1, pregnant, or if other comorbidities exist, if available. Hepatitis A vaccine should be offered to contacts if IG Is not available. The dosage of IG is 0.1mL/kg. 3,4,5
- Consider helping with the local efforts. There are various ways to do this:
- Join the Medical Reserve Corps (MRC). Though some paperwork is required to be completed up front (background check), once you become a member, you can respond with any of the LMPHW efforts that are already ongoing. Joining the MRC does not obligate you to respond to future events. If you are interested in joining the MRC, please contact Kim Rogers at (502) 526-6833.
- Work with your organization to spread the word of the outbreak and encourage involvement in response efforts. We all have competing priorities within our own organizations and having physician champions for this cause can help highlight this as a priority in your organization. If you are a leader within your organization, consider how you could assist in our outbreak response. Kentuckiana Health Collaborative members can help by ensuring the populations under their care receive vaccine. Increasing communications with those within their organization on how they can receive the vaccination is instrumental in this process.
- Identify additional locations where vaccination may be needed. If you are involved in community organizations or events that serve at-risk populations, let us know! We have found many locations such as churches and food pantries that have allowed us to reach those with vaccine that we might not have reached otherwise.
- Donate money or items to help with vaccine efforts. Thank you to those partners who have already been generous donors, including Anthem, Aetna, and the many businesses who have provided immunizations for their workers.
For more information or to get involved in the HAV outbreak response, please contact us at Sarah.Moyer@louisvilleky.gov or Lori.Caloia@louisvilleky.gov.