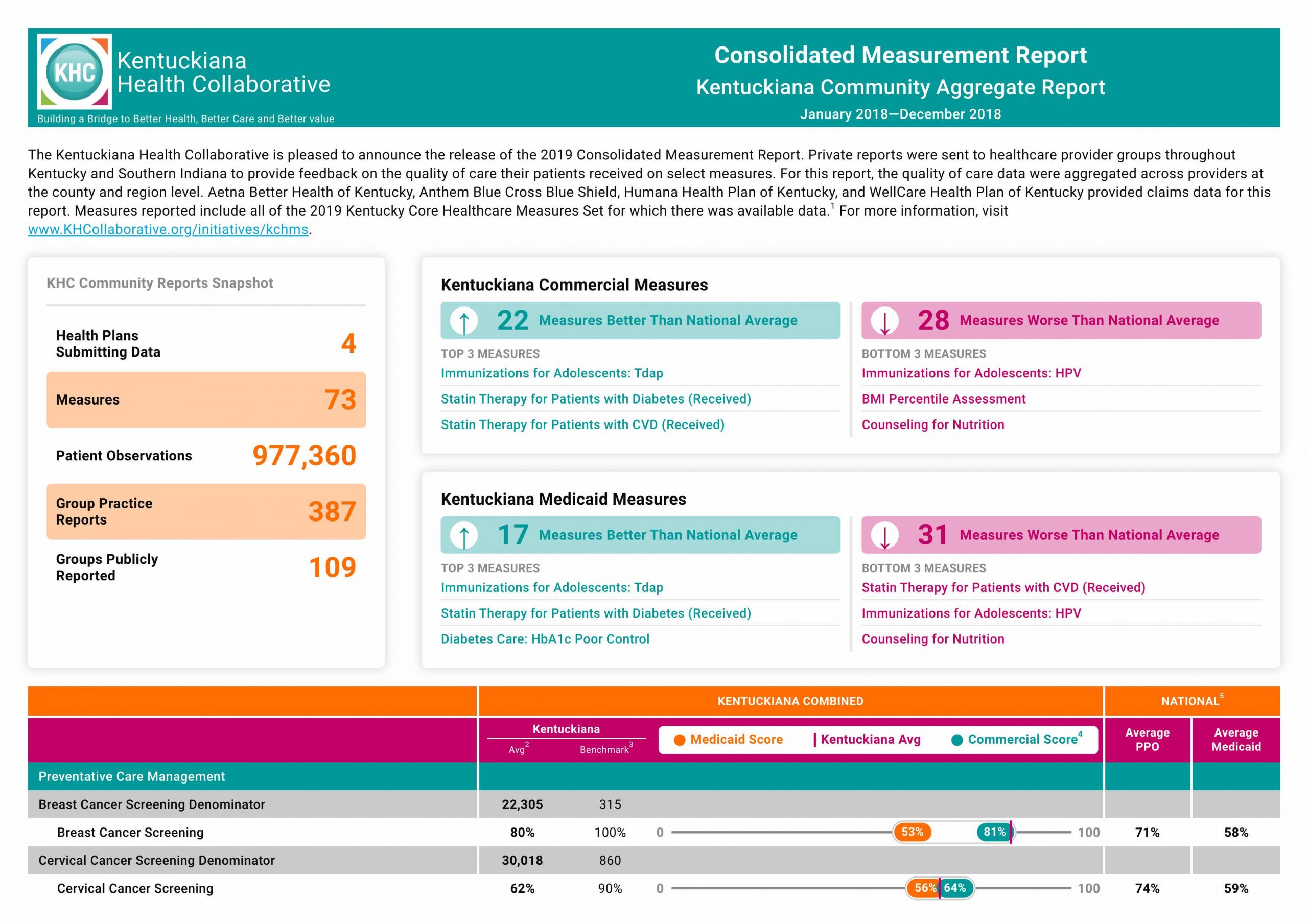
In April, the Kentuckiana Health Collaborative sent private reports to nearly 450 group practices throughout Kentucky and Southern Indiana. Soon after, the KHC released its annual community reports, featuring highlights of where the community performs well and where there are gaps in care.
On Thursday, the KHC held a webinar introducing the 2019 community reports and diving into some of those highlights. If you missed it, you can access the recording here. As a community, Kentuckiana and the Commonwealth have seen an improvement in historical trouble spots, we have new information on opioid prescribing, and there are opportunities for growth and exploration in some new measures.
IMPROVEMENTS IN DIABETES CARE AND VACCINATIONS, OPPORTUNITIES FOR GROWTH IN NUTRITION COUNSELING
I encourage you to go to our website and look through the reports yourself. Once you account for age stratifications or multiple rates per measure – such as antidepressant medication, which has two rates, for acute period and continued period of treatment – there are 73 total measures to have fun with. You can access the full reports here.
Retinal eye exams for individuals is an area where we have traditionally fallen woefully short. Left unmanaged, diabetes can lead to serious complications, including blindness. In Kentucky, diabetes is the leading cause of blindness. For more than the last decade, Kentucky fell in the low-40% range, far below national averages, which tended to be in the mid to high 50s. The KHC has done quality improvement projects in the past on this critical aspect of care, as have many organizations across the state.
But in the last couple of years, as you can see, we have improved pretty spectacularly. In fact, we are above national rates for commercial AND Medicaid!
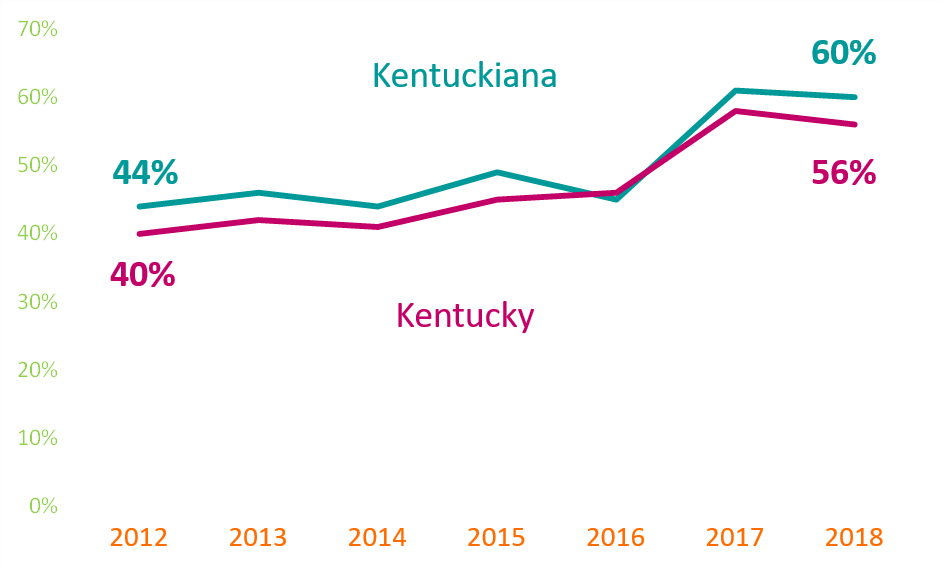
This is a perfect example of why we need quality reporting like this. Without knowing where we stand, we wouldn’t be able to know where to focus our efforts and resources. Additionally, we are often surprised when we assume we do well in things that the data tells us the opposite, and vice versa!
Another area that Kentucky continues to improve is in a relatively new focus area of HPV vaccination. This measure only became part of the HEDIS program in 2017 (using 2016 data), and the Kentucky Core Healthcare Measures Set committee selected it as a high priority, recognizing that Kentucky has the highest rate of HPV-related cancers.
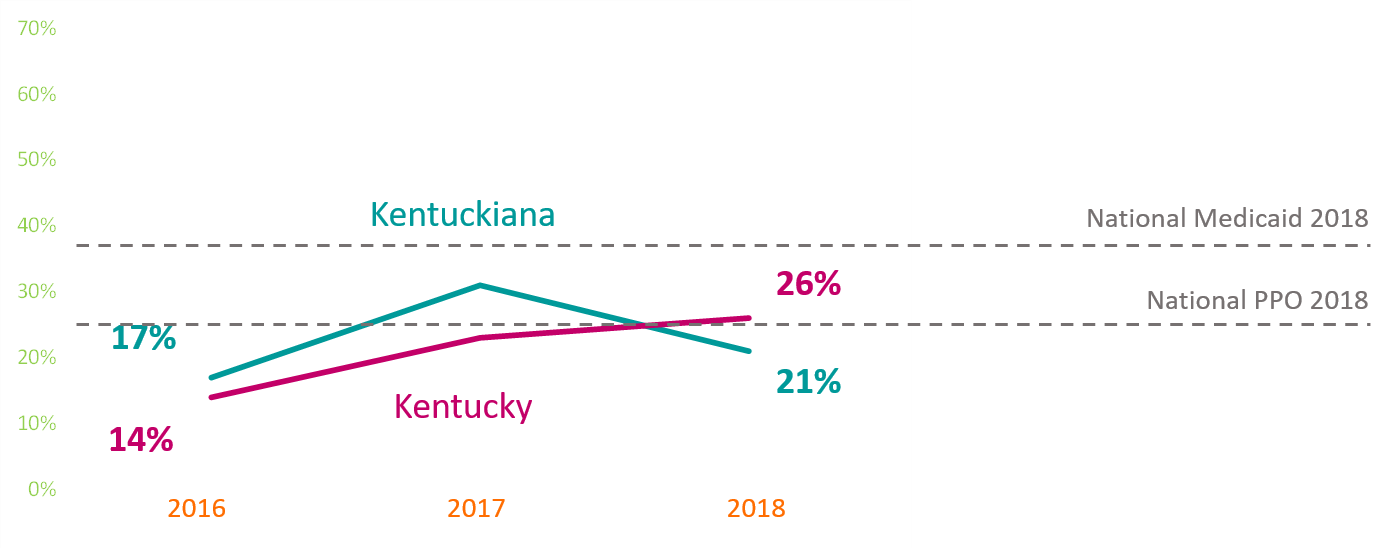
Unsurprisingly, when our first baseline year of data came in, Kentucky and Kentuckiana fell below the national rates. But in our third year of reporting, Kentucky has made double digit improvements. Anecdotally, it seems like providers are getting more and more comfortable talking to patients and patients’ parents about HPV and making it a part of routine adolescent immunizations.
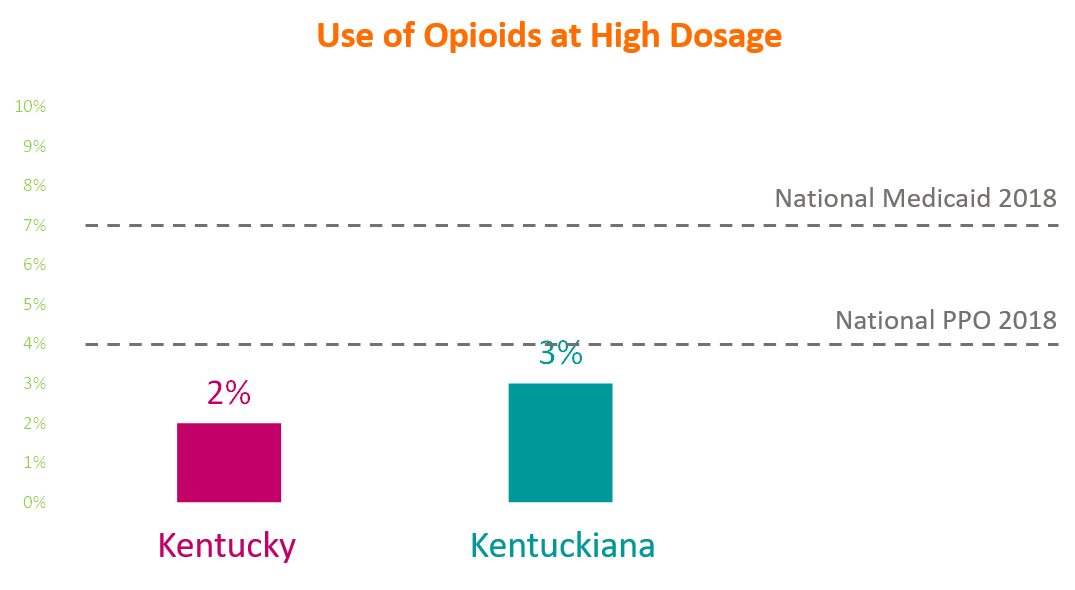
As you might be aware, a big focus in the past few years has been appropriate opioid use, as part of a partnership with the Kentucky Opioid Response Effort, as part of a SAMHSA Grant awarded to the Kentucky Cabinet for Health and Family Services. We have two new measures related to this work – use of opioids at high dosage and use of opioids from multiple prescribers.
For all opioid measures, lower is better. So the graph below that shows regional and state rates lower than national commercial and Medicaid rates is a good thing. A smaller proportion of Kentucky’s patients received high dosages of opioids in 2018 than the rest of the nation.
Another new measure to this year’s reports you will notice is all over our “areas for improvement” section at the top of the reports: Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents.
There are three rates in this measure – BMI percentile documentation, counseling for nutrition, and counseling for physical activity. This was a huge topic of discussion for the Pediatric Committee on the core measures set team. While any measure that includes counseling can be tough for a provider to “get credit for,” the committee, about half of whom were pediatricians, felt strongly that this is the crux of the work they do – providing the foundation for a lifetime of healthy habits – and wanted it included, despite the challenges.
Since many of these pediatricians felt like they were doing this well to begin with, they saw it as an opportunity to “get credit for” the good work they’re already doing. By focusing on documentation improvements and practice flow, they feel we can make great progress as a state in this measure.
The last measure I wanted to highlight to you actually will not see on the 2019 KHC Community Reports. Part of the Comprehensive Diabetes Care set, that includes eye exams, foot exams, and HbA1c poor control, Blood Pressure Control is a measure new to the Kentucky Core Healthcare Measures Set, so this year was the first year we collected data for it.
But you won’t see it on the reports, because we are still establishing a baseline for that data and seeking to understand what the data is telling us. Information for this measure is usually recorded by providers in the medical record data and typically not administrative data. If a provider bills a CPT code that is <140/90, the data could be captured administratively but that does not typically occur. So that’s why we see a wide range of results. We are looking into how to best use this data and work on this measure. Stay tuned for more information!
COVID-19 AND ITS IMPACT ON QUALITY MEASUREMENT
Already, there have been major changes to the 2020 NCQA HEDIS program reporting requirements, and it seems like every day, more things are changing. Much is unknown right now. NCQA has a webpage dedicated to the pandemic that I encourage everyone to visit for more information. Of course, while HEDIS is the program we most closely work with at the KHC, it certainly isn’t the only one. CMS’s Medicare quality reporting programs have granted a variety of exceptions and extensions to providers for reporting.
However, despite all of these changes, we don’t expect a delay in our KHC 2020 reports. Changes to the HEDIS program primarily affect hybrid measures, measures that combine administrative claims data and medical chart reviews, and the measures that the KHC collects use just administrative data. We’ve been having one-on-one meetings with our health plan partners, as well as our KHC Measurement Strategy Team, and haven’t heard of any concerns for submitting data for the KHC annual reports.
It is still too early to tell, but I expect big changes in measurement programs for next year. Preventive care has already seen a big impact, as has medication access and adherence for chronic conditions, etc. Efforts around telehealth services and behavioral health services, which were already large areas of focus, have been a big area of discussion. Many expect these efforts to be ramped up in response to the pandemic. Health plan partners have also been addressing social determinants of health, such as food insecurity, as a result. Again, these plans were already working in these areas, but have been forced to scale those programs and pilots in a compressed time span.