Prevention
Prevention involves measures to avoid misuse and dependence by reducing medical and non-medical exposure to opioids. Prevention of developing complications once a person has developed addiction can also include harm reduction services that aim to reduce the likelihood of negative consequences or death as a result of opioid use. These can include needle exchanges and naloxone for overdose prevention.
Treatment
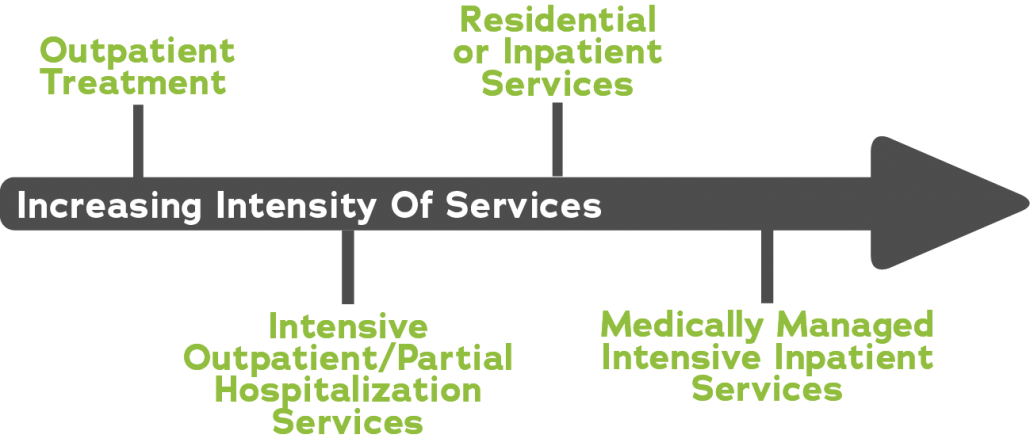
Treatment involves diagnosis and professional treatment of individuals with OUD. Evidence-based treatment for OUD can involve several treatment modalities that address biological, social, and psychological issues within the individual. This includes Medication for Opioid Use Disorder (MOUD) and individual and family behavioral therapies. These modalities can be supplemented by recovery support services. As defined through the American Society of Addiction Medicine (ASAM) criteria, treatment can be carried out on a variety of inpatient or outpatient levels, depending on the individual’s situation, substance of use, and required intensity of care.
MOUD, commonly referred to as Medication Assisted Treatment (MAT), is more effective in reducing illicit opioid use, keeping people in treatment, and reducing risks of overdose than in treatment without. There are three types of approved medications: methadone, naltrexone, and buprenorphine. These three drugs are available under a variety of brand names as approved by the Food and Drug Administration (FDA). Each of these medications works differently, presenting their own risks and benefits, and should be discussed and made available to treat anyone diagnosed with OUD. It is important to note that the use of prescribed FDA-approved MOUD as part of treatment is consistent with the definition of abstinence.
MOUD can be supplemented with behavioral therapies or counseling. Behavioral therapies and counseling services for OUD can help change attitudes and behaviors associated with use, build healthy life skills, and support adherence with other forms of treatment. It can be provided by physicians as part of an individual’s medical visit, but some people may require or benefit from specialized counseling services provided in individual or group settings. This counseling can be offered to individuals who are using opioids, as well as their friends and family.
Another potentially helpful supplement to treatment is recovery support services. These services are not clinical in nature but are often provided by trained volunteers or other people who are in recovery. These supports include assistance with navigating systems of care, removing recovery barriers, staying engaged in the recovery process, and providing a source of community.
People with OUD should have access to all of these services at all levels of treatment, allowing them to find the approach that best fits them. However, there is strong science for supporting the effectiveness of MOUD, and it should be considered as the status quo for treatment.
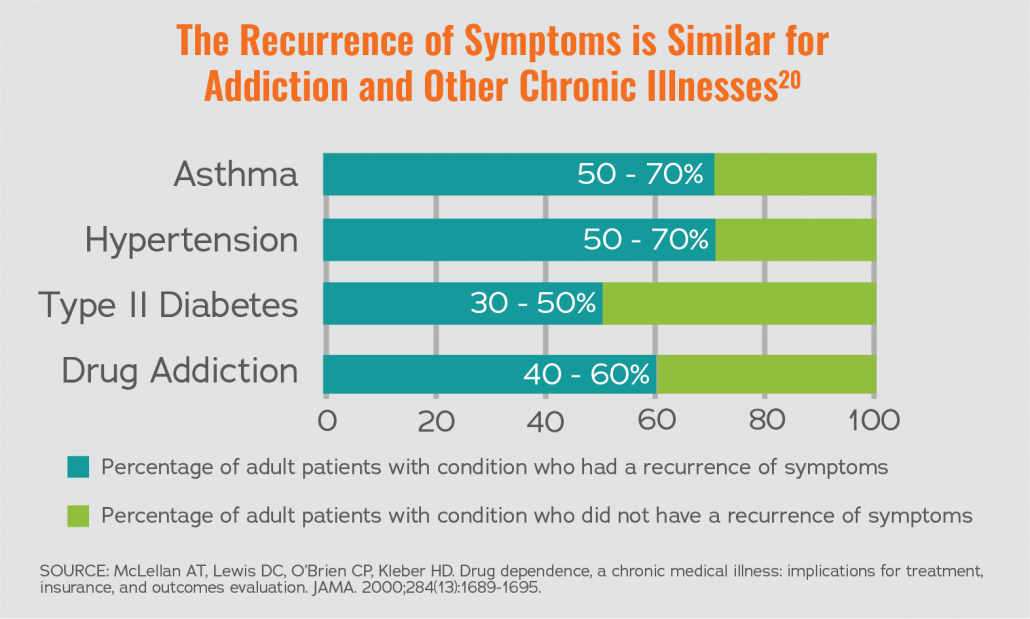
Remission is the goal of medical treatment for chronic disease and involves the person having no signs or symptoms of active disease. While remission is a goal, people with chronic diseases often have periods of worsening symptoms. People who are actively in treatment may not be in remission at all times. Since OUD is a chronic disease, people often need ongoing care at some level.
Recovery
Unlike acute illnesses, recovery for a person with a chronic disease involves active ongoing self-management that often requires the help of biological, psychological, and social supports. The Substance Use and Mental Health Services Administration (SAMHSA) defines recovery as “a process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential.” The process of recovery is a very personalized process that is built on the individual’s own characteristics and resources and is a much broader concept than medical remission for any chronic disease.